What is Insulin Resistance?
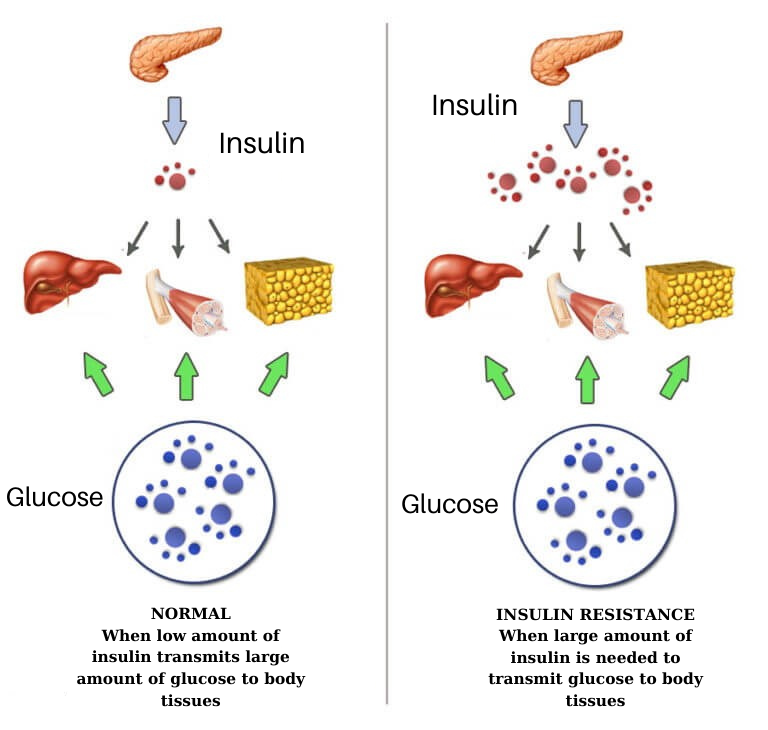
Insulin resistance can be defined as the difficulty in showing the effect of insulin in the body despite the adequate secretion of insulin hormone, or the failure of biological events to stimulate.
What is Insulin? How It Functions?
Insulin is a hormone secreted from the pancreas. Its main effect is to lower the blood glucose level and enable the intake and use of glucose in tissues that use blood glucose such as fat, muscle and liver.
Insulin hormone is secreted from beta cells in the islets of Langerhans of the pancreatic gland located under the stomach. Insulin secretion from the pancreas is regulated according to the blood glucose level. When blood glucose increases, rapid insulin secretion occurs within the first 1-2 minutes, and this is called "first phase insulin secretion". This secretion lasts 3-7 minutes. Then, the secretion called the second phase occurs, which is a slow secretion and is continuous.
Daily insulin production in a healthy adult with normal weight is approximately 40 ± 8 IU. In people with normal metabolism, insulin secretion increases in response to the rise in blood glucose. A small increase in blood glucose level of 10 mg/dl stimulates insulin release. In the first 15 minutes following oral food intake, the level of insulin in the blood increases rapidly.
The amount of insulin is described as "international unit (IU)”. An IU of insulin is defined as the amount of insulin that lowers blood glucose from 120 mg/dl to 45 mg/dl in a 2-kg rabbit fasted for 10 hours. In humans, the amount of blood glucose decrease with 1 IU insulin varies from person to person.
In healthy individuals without diabetes, normal physiological insulin secretion occurs in two ways:
- Basal Insulin: It is the insulin secretion that meets the need during the hours outside the meal and at night when the blood glucose does not rise very much. It is secreted at the ratio of individuals' needs, especially in the late hours of the night, it shows a slight increase to suppress glucose output from the liver (hepatic glucose output).
- Bolus (Prandial) Insulin: It is the release of insulin triggered by the increase of other substances such as glucose or amino acids in the blood following a meal. Following bolus insulin release, blood insulin levels (fluctuations) vary according to the carbohydrate amount and content of the meal. Normally, bolus insulin secretion reaches its peak 20 to 30 minutes after a meal is eaten and returns to basal levels within 2 hours.
Why Does Insulin Resistance Occur?
In order for insulin to be effective in the body, it must bind to the receptors on the cell membrane, enter the cell and show its effect. When insulin resistance occurs, the cell becomes unresponsive to insulin in the environment. Conditions that prevent insulin from binding to the receptors or reduce its effect after binding cause insulin resistance. Many different metabolic changes and disorders may play an important role in the development of insulin resistance.
Who Develops Insulin Resistance?
What Are the Risk Factors Composing Insulin Resistance?
- Genetic predisposition
- Obesity,
- Enlarged waist circumference,
- Hypertension,
- Polycystic ovary syndrome (PCOS),
- Sleep disorders such as sleep apnea,
- Aging,
- Sedentary lifestyle,
- Diet,
- Smoking,
- Use of various medications,
can cause insulin resistance.
Apart from these;
- Ovarian cysts,
- Excessive or insufficient growth hormone,
- Excessive secretion of cortisol and adrenaline hormones in response to stress,
- Excessive prolactin
- Excessive or insufficient functioning of the thyroid gland,
- Parathormone elevation,
- Deficiencies of male and female hormones,
- Gestational diabetes
- Cushing's Syndrome,
- Acromegaly
can cause insulin resistance.
What Are the Symptoms of Insulin Resistance?
How Is Insulin Resistance Diagnosed?
The measures that allow to understand the presence of insulin resistance are:
- Waist circumference longer than 102 cm in men and 88 cm in women,
- Having a body mass index over 30
- Decreased HDL (good cholesterol) (below 40 mg/dl in men, 50 mg/dl in women),
- High triglyceride (over 150 mg/dl),
- Elevated fasting blood glucose (over 100 mg/dl),
- High blood pressure (130/80 or higher),
- Signs of hypoglycemia
The presence of 3 of these criteria in a person is called Insulin Resistance Syndrome or Metabolic Syndrome, regardless of insulin level.
Insulin Resistance Test
Apart from the above-mentioned measurements and laboratory results, the person may also suspect the presence of insulin resistance by questioning daily routine:
- Difficulty in concentrating, instability, headache or somnolence after meals,
- Tremors in hands after meals, cold sweats,
- Having hunger pangs,
- Getting hungry quickly, feeling full late,
- Sudden and frequent desire to eat desserts and pastries,
- Uncontrollable weight gain,
- Fatigue,
- The gradual enlargement of the waist circumference,
- Dark, velvety skin browning, especially in the armpits, groin, neck areas, called acanthosis nigricans,
- Menstrual irregularities in women
Also, family history of overweight and diabetes is one of the signs of insulin resistance, and an endocrinology or internal medicine specialist should be consulted.
Diagnosis of Insulin Resistance
How Is Insulin Resistance Diagnosed?
In the evaluation of the metabolic status associated with insulin resistance, the diagnosis can be made with the patient's complaints, physical examination findings and simply measuring waist circumference. However, in some cases, additional tests may be ordered to determine the risk of diabetes.
Fasting blood glucose test (fasting plasma glucose), glucose loading test (oral glucose tolerance test) and HbA1c test that shows the average blood glucose level over the last 2-3 months are among the tests that may be requested. In addition, some data such as blood lipids and liver enzymes can be helpful for diagnosis.
Although there are many different methods for calculating insulin resistance, HOMA-IR, HOMA for Homeostatic Model Assessment and IR for Insulin Resistance, calculation method is widely used and preferred. In addition to insulin resistance, this test also provides information about the functions of cells that have the ability to produce insulin from the pancreas. Insulin resistance can be detected in people whose HOMA score is higher than 2.5. However, it may not be necessary to measure the HOMA value in every patient. Waist circumference is the best parameter to show insulin resistance in clinical practice.
Treatment of Insulin Resistance
Lifestyle changes and regular exercise can improve insulin resistance in the vast majority of patients. A low glycemic index diet (foods that do not raise blood glucose or raise it slowly) is very important. In cases where insulin resistance cannot be controlled with lifestyle changes alone, some medications may be prescribed by the physician to keep blood glucose under control. Regular exercise and weight loss are the most important factors that decrease insulin resistance. Only with exercise and healthy nutrition, 60% of insulin resistance can be corrected.
There is no magic nutrient or supplement that will instantly fix insulin resistance. Instead, it's important to constantly change what you eat and focus on foods that contain as much vitamins, minerals and fiber as possible.
What Happens If Insulin Resistance Is Not Treated?
What Diseases Does Insulin Resistance Cause?
Insulin resistance is the most important cause of prediabetes. Prediabetes is a health condition in which the blood glucose level is higher than normal but not yet high enough to be diagnosed as Type 2 diabetes. Prediabetes is defined as the period before becoming diabetic and impaired glucose regulation.
Insulin resistance is higher in overweight people, as the weight increases, this resistance increases accordingly as well as the likelihood of diabetes. Especially the accumulation of fat in the abdomen around the internal organs increases the risk of diabetes.
The increase of soluble fatty acids in the blood both impairs the functioning of insulin and the storage of these fats in tissues such as the pancreas and also contributes to the development of diabetes.
Excessive or low levels of hormones such as leptin, adiponectin, and TNF-alpha secreted from adipose tissue also contribute to the development of diabetes.
Unless insulin resistance is treated, high blood pressure, high triglyceride (blood fats), high uric acid, steatosis around abdomen, hepatosteatosis (fatty liver), tendency to have blood clots, decrease in HDL cholesterol (good cholesterol) and increase in urinary protein (microalbuminuria) may occur together.
Excessive insulin circulating in the blood creates a suitable environment for the development of chronic diseases such as;
- Obesity,
- Type 2 diabetes,
- Hypertension,
- Stroke,
- Atherosclerosis,
- Elevated lipid,
- Ovarian cysts (polycystic ovary syndrome),
- Hepatosteatosis,
- Infertility,
In recent years, studies show that insulin resistance are seriously correlated with:
- Colon cancer,
- Bile duct cancer,
- Esophageal cancer,
- Ovarian cancer,
- Uterine cancer,
- Breast cancer,
- Prostate cancer,
- Bladder cancer,
- Kidney cancer,
- Thyroid cancer,
- Lymph cancer
There are also studies that found a link between Alzheimer 's disease and insulin resistance.
Insulin resistance accelerates the aging process by disrupting the body's metabolic and hormonal balance.

